Table of Contents
How Colonoscopy Preparation Affects the Gut
Why Bacillus subtilis and Enterococcus faecium Work Well
What Studies and Clinical Observations Reveal
Mechanism of Action of Probiotics in the Gut
Who Hires Most from These Probiotics?
How to Take Probiotics After a Colonoscopy
Introduction
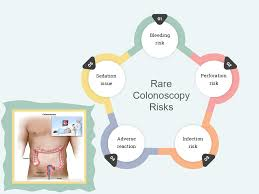
Among the currently available diagnostic and therapeutic methods in medicine, colonoscopy is the most significant one. In essence, through such an operation, specialists would be able to find polyps, inflamed areas, and precancerous colon tissues. In contrast to the procedure, which is safe and regular, the preparation for bowel cleansing would bring drastic changes to the gut balance. To top it all, the transient improvement of gut microflora usually causes symptoms like bloating, irregular bowel movements, abdominal pain, and a gut feeling of “not back to normal,” which is typical for the whole set.
The recent research findings, as clinical evidence, lead to a potentially effective intervention: the prompt intake of the probiotics Bacillus subtilis and Enterococcus faecium after colonoscopy. Those people who use such targeted probiotic strains not only get a better recovery of well-adapted gut microorganisms in their intestines, but they also seem to achieve an earlier improvement of gastrointestinal symptoms as compared to the placebo group. It implies that probiotic supplementation is a significant post-surgical application that can help speed gut health rehabilitation.
How Colonoscopy Preparation Affects the Gut
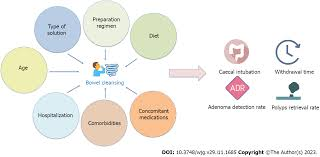
To perform a colonoscopy, patients must actively empty and cleanse their colon.
This is essential for a clear view; thus, it not only gets rid of all the waste but also removes a significant (though not the entire) part of the gut microbial populations.
This process kills the good bacteria. For a certain period of time, the intestinal tract is devoid of bacteria that support digestion, immunity, and nutrient absorption.
Very fast decreases in microbial diversity turn the gut into a weak organ.
Some of the common symptoms after a colonoscopy are
Bloating with gas
Slower or irregular bowel movements
Cramping
Increased sensitivity
Temporary absorption of nutrients issues
However, all these symptoms disappear, but each has a different recovery duration. Some may take days; others will take weeks before the gut can function normally again. Therefore, the advantage of these particular probiotics becomes obvious.
Why Bacillus subtilis and Enterococcus faecium Work Well
Not every probiotic is equally efficient in providing post-colonoscopy support. The properties of Bacillus subtilis and Enterococcus faecium are exceptional for two main reasons:
1. After staying in the acid-resistant part of the stomach, they come to the intestines alive. One of the main causes for the reduced effectiveness of probiotics is their death in the acidic environment of the stomach, which happens to most of them.
On the other hand, as a spore-forming microorganism, Bacillus subtilis is naturally shielded and can go to the large intestine without being harmed. Enterococcus faecium is also very resistant to stomach acid and bile.
2. They swiftly bring about microbial repopulation.
Once patients empty their gut, it becomes an open space ready for colonization. Using these two strains, the colon will not only…
Help beneficial entity reproduction
Push out harmful organisms
Microbial diversity restoration
Strengthening the integrity of the intestinal wall
3. Improvement in digestive symptoms.
Taking these probiotics together, people say that they experience:
Less bloat
More regular bowel flow
Less cramping
More rapidly, overall, digestive comfort
People taking probiotics tend to see these effects earlier than those who don’t.
What Studies and Clinical Observations Reveal
All patients who were administered Bacillus subtilis and Enterococcus faecium after a colonoscopy increasingly demonstrate more advantages of these bacteria over the placebos. This is supposed to happen within a few days of treatment, indicating a rapid microbial rebalancing.
Moreover, patients confirm that their gastrointestinal symptoms improve earlier. Intestinal discomfort that is temporarily experienced and may last up to several days without intervention is often significantly shorter in duration.
So, rapid microbial restoration, along with symptom relief, makes such probiotics the best choice for the post-colonoscopic phase.
Mechanism of Action of Probiotics in the Gut
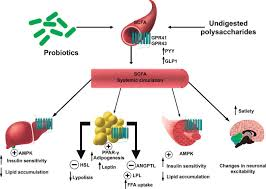
1. Broadening Microbial Diversity
The human gut depends on a large number of species for its health.
The insertion of Bacillus subtilis will serve as a “starter culture,” facilitating the growth of other beneficial bacteria.
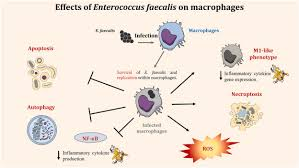
The contribution of Enterococcus faecium to the regulation of intestinal flora balance and fighting harmful microbes is very active.
2. Improvement in transpapillary lining integrity
Sensitivity in the colon lining after the cleansing is enhanced by clarity.
With mucosal integrity enhancement, these probiotics turn the gut lining into a more resistant one.
3. Immunopotentiating Function
Most of the immune system (70%) is located in the gut, so the restoration of bacteria would mean the restoration of immune balance after a colonoscopy.
4. Reduced Gas and Fermentation
By giving an effect of decelerating the fermentation processes, these two strains lead to lowering the production of excessive gas and thus, relieving bloating.
Who Hires Most from These Probiotics?
Quite possibly every person on whom a colonoscopy is performed would gain from these probiotics, particularly those who:
Experience bloating and discomfort after the bowel cleansing
Have a history of digestive sensitivity
Just wrapped up antibiotic treatment
Have a diet low in fiber-rich foods
Feel their microbiomes recover slowly
Unless a healthcare provider gives other directions, any adult can take them.
How to Take Probiotics After a Colonoscopy
Most experts’ best recommendation:
Immediately after the operation, begin.
Continue this for a minimum of 7–14 days.
Usually, probiotics are consumed with water, preferably on an empty stomach.
The probiotic most ideal according to the majority of people is the one that specifically lists Bacillus subtilis and Enterococcus faecium.
Final Thoughts
Along with a short-term inconvenience, the possible positive effects on long-lived health via colonoscopy come coupled with the temporary disruption of the gut microbiome. These are the probiotics with Bacillus subtilis and Enterococcus faecium from which the patient recovers, simply and effectively, naturally, and without any intervention, from all possible sources. This is good because healthy bacteria will return earlier, and some of the digestive symptoms will be relieved much faster, thus making the overall experience much easier and more comfortable after the procedure.

Leave a Reply