Table of contents
Microstructure of White Matter in Bipolar Disorder
The neural mechanism of white matter change
Closing Remarks and Future Directions
Future directions for research include:
Introduction
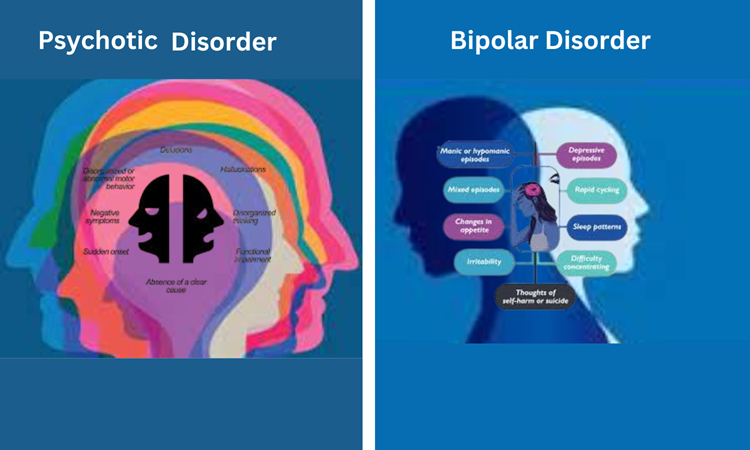
Bipolar disorder (BD) is a complex mental health condition characterized by episodes of debilitating mood swings and cognitive impairment, and in some cases, psychosis. Having a lifetime prevalence of about 1% globally, BD represents a great burden on patients, families, and healthcare systems. With recent advances in neuroimaging and genetics, the neural correlates of BD have begun to be elucidated, with special focus on white matter microstructure. Through these findings, the article assesses the connections between white matter changes, psychotic symptoms, and BD and discusses the implications for personalized treatment and research redirection.
Microstructure of White Matter in Bipolar Disorder

White matter, which is made of myelinated axons, helps in communication between brain regions. Changes in white matter microstructure have been associated with multiple psychiatric disorders, including BD. Meta-analyses have shown that BD patients have decreased white matter integrity and have consistently reported decreased integrity in the anterior limb of the internal capsule, the anterior cingulate cortex, and the superior longitudinal fasciculus.
Psychosis and the Widespread Microstructural Impact on White Matter

Psychosis is one of the key features of BD and refers to a detachment from reality, commonly experienced in hallucinations or delusions. Research indicates that psychosis might be linked with more significant changes in white matter microstructure. A recent study reported a decreased fractional anisotropy (FA) of the corpus callosum, anterior cingulate cortex, and superior longitudinal fasciculus in BD patients with psychosis compared to those without psychosis.
The neural mechanism of white matter change

The precise neural basis of white matter changes in BD, however, remains unknown. But there have been a few theories that have been suggested:
Neuroinflammation: Long-term neuroinflammation might lead to the loss of integrity of the white matter and disturbance of neuronal connections.
Oxidative stress: Myelin damage and degeneration secondary to oxidative stress can lead to impaired integrity of white matter.
Genetic strengths: Genetic differences, such as myelin-related genetic changes, might play a role in white matter changes in B.
Closing Remarks and Future Directions
The insights of this study are clinically very relevant:
Early diagnosis: White matter alterations in BD patients could have been useful in early diagnosis and treatment.
Individualized therapy: Elucidating the neurobiological mechanisms that underlie white matter changes could lead to the inception of individualized therapeutic approaches.
Monitoring disease evolution: Factors measuring white matter molecules over time in longitudinal studies may help to understand how the disease evolves and the effectiveness of treatments.
Future directions for research include:
Integration of neuroimaging and genetics: Joint analysis of neuroimaging and genetic data may lead toward a better understanding of the neural pathways involved in BD.
Finding new treatments: Some research may target novel treatments that focus on neuroinflammation or oxidative stress.
Bipolar disorder (BD), Psychosis as a potential confounding factor: Further studies are required to clarify the relationship of psychosis and alterations in white matter in BD.
Conclusion
White matter pathways are important, as they mediate communication between brain regions and play an important role in building neural circuitry that is disrupted in bipolar disorder. We reviewed the literature reporting on white matter abnormalities in BD and psychosis and discussed their potential relationships, calling for more precise interpretation of the findings in the context of BD and psychosis, as well as the evolution to studies using more personalized treatment and other exploratory approaches to assess the role of white matter alterations.
References:
Merikangas, K. R., et al. (2011). World Mental Health Survey Initiative: Lifetime Prevalence of Mental Disorders in the World. World Psychiatry 10, 168–176 (2011).
Benedetti, F., et al. (2011). V. White matter lesions in bipolar disorder. Journal of Affective Disorders, 131(1–2), 155–162.
Baryshnikov, B. V., et al. (2017). A systematic review and meta-analysis of white matter microstructure in bipolar disorder. Journal of Affective Disorders 209, 101-111.
Wang, Y., et al. (2020). Altered white matter in patients with and without psychosis in bipolar disorder. Journal of Psychiatric Research, 123, 102–109.
Berk, M., et al. (2011). A meta-analysis of bipolar neuroinflammation: A systematic review. 31(5), 653-656. {{Cite journal|author=Kipnes|journal=Journal of Clinical Psychopharmacology|month=October|doi=10.1097/01.jcp.0000230654.03237. Andreazza, A. C., et al. “Cerebrospinal Fluid Levels of Glutamate in First Episodes of Psychosis.” a8|issue=5|pages=653–656|year=October 2008|pmid=18813142}} (2013). Atherton, K. J., & Niven, H. L. (2013). Oxidative stress and mitochondrial dysfunction in bipolar disorder. Journal of Psychiatric Research, 47(11), 1723–1731.
Goes, F. S., et al. (2012). Bipolar disorder (genome-wide asso
Leave a Reply