Table of content
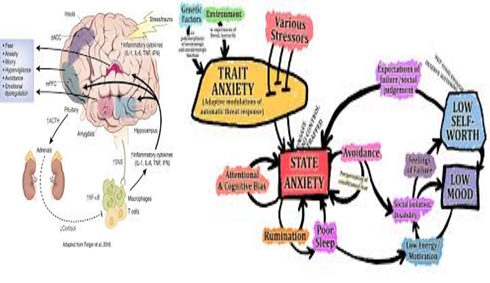
What falls on the Anxiety spectrum?
Generation Gap- A New Way of Being Effected
Anxiety has effects on functioning and development
Digital and low-intensity interventions
Neurosurgery and newer modalities
Neurosurgery and newer techniques
The future of tailoring care for generations to come
Introduction
Anxiety disorders may vary from a GAD of chronic low-grade worry in one person to hyper-aroused intrusions in memory in PTSD in another person. Within the last decade, clinicians and researchers have noted modifications in anxiety’s clinical presentations and youth impact. While social, technological, and global stressors shape risk and recovery, treatment modalities are now most variable through taking on board digital, brain stimulation, and trauma-oriented approaches, in addition to the conventional pharmacological and psychotherapy.
This article covers the anxiety spectrum: GAD: Being in a constant state of nervousness, with excess worry to several life domains (work, health, money), hence interfering with normal functioning.
What falls on the Anxiety spectrum?

Generalized anxiety disorder (GAD): The persistent concern about multiple areas of life – work, health, money – interfering with daily functions. Symptoms include nervousness, weakness, irritability, great difficulty concentrating, muscle tension, and sleep.
Panic disorder: Recurrent panic attacks (fear and anxiety with palpitations and breathlessness among others); also worry about further attacks generally sets in.
Social anxiety: Judged or embarrassed in social or performance situations is a marked anxiety.
Specific Phobias: Unreasonable fear far above proportion to a stimulus or situation- for example heights, needles, etc.-with avoidance usually being the preferred response
Post-Traumatic Stress Disorder (PTSD):
PTSD initiates with a set of symptoms after experiencing a traumatic event that comprises intrusions, avoidance, negative mood/cognitions, and hyper-arousal.
Other anxiety-related conditions: Other anxiety-related conditions (which can sometimes present as obsessive-compulsive disorder) are adjustment disorders with anxious features; other anxiety-related issues.
Anxiety is never categorized by a given diagnostic box. Most often, any form of anxiety would coincide with depression, substance use, or otherwise.
Generation Gap- A New Way of Being Effected
Some present forces which influence anxiety on youth:
1. Digital life and social networks: This is where the permanent exposure to an edited, curated environment, comparison culture, cyberbullying, and informations overload becomes fueling self-negative appraisals and social anxiety. The instant feedback (likes, comments, etc.) only makes it worse in terms of rejection sensitivity.
2. Academic-economic pressure: More competitive education, concerns regarding student debts, and an even more precarious job-market situation increase other chronic anticipatory stressors that feed GAD in human beings.
3. Global crises and uncertainty: Climate anxiety, political instability, and the COVID-19 pandemic have created a climate of collective trauma and grief, with a nagging sense of unpredictability, making matters worse for GAD and for trauma-related presentations.
4. Sleeping disturbances and lifestyle: Erratic sleep patterns as a result of late-night gadget use reduce the ability to regulate emotions while making one susceptible to anxieties.
5. Increased awareness and reduced stigma: In a paradoxical way, greater diagnosis is actually the sign of greater awareness and willingness to come forward for help.
6. In early life stress and adverse childhood experiences:In early life stress and adverse childhood experiences (ACEs), one consequence is that childhood risk factors significantly increase the lifetime risk for anxiety and PTSD; moreover, parenting styles have relevance as well.
The aggregation effect: A large number of youths experience a comorbidism of mixed chronic, functionally impairing anxiety that obstructs their pathway through education, future relationships, and identity formation.
Anxiety has effects on functioning and development
Cognitive: Worry and hypervigilance impede focus working memory and school performance.
Social development: Isolation from any people will not support making friendships and learning other skills.
Emotional well-being: Anxiety in its extreme often extends to depression, substance use, or suicidal ideation.
Physical health: Stress with the lowered immune function presents as headaches, digestive problems, and sleep issues.
Career path: Unfulfilled potential and below-par performance, thanks to some early disruptions at the career threshold.
Essentials of assessment
Assessment comprises a combination of taking histories, inventories of symptoms (such as GAD-7 for GAD or PCL-5 for PTSD), observing behavior, and getting collateral information from family, school, or employers. Exploring trauma history and establishing suicidality are extremely important. What also needs to be considered is whether functional impairment is severe or mild, as this will guide their urgency for treatment.
Evidence-Based Interventions

Psychotherapies most often used to intervene in cases of anxiety disorders.
Cognitive Behavior Therapy (CBT): Rewiring of maladaptive cognitive-attitudinal processing and avoidance behavior. It is the behavioral arm of CBT which constitutes Exposure, which is the gold standard in the treatment of phobias and social anxiety as well as panic disorder and mixed trauma-related symptoms. Trauma-focused interventions as geared towards the treatment of PTSD include:
– Prolonged exposure (PE): Systematic controlled exposure to trauma memories and avoidance situations to reduce fear.
– Cognitive Processing Therapy (CPT): Changes in impaired trauma-related beliefs.
– Eye-Movement Desensitization and Reprocessing (EMDR): A method of reducing distress which is highly advantageous for persons with PTSD. It involves bilateral stimulation in association with remembering trauma.
– Acceptance and Commitment Therapy (ACT): Uses action based on values and acceptance of difficult emotional states instead of symptom reduction. Interpersonal Therapy (IPT) & mindfulness-based interventions.
Medication
Selective Serotonin Reuptake Inhibitor (SSRIs) and SNRIs: These are first-line agents of pharmacotherapy for chronic anxiety disorders and PTSD, as in fluoxetine, sertraline, escitalopram, and venlafaxine.
Benzodiazepines: Even used in the short-term management of intense panic, risks depend on development of physical dependence and loss of possible gains from treatment; caution is thus exercised while clinicians use.
Adjuncts: Prazosin for trauma-mechanism nightmares; atypical antipsychotics in some cases are used as augmentation for those that fail to respond.
Medication choice is further determined by the severity, age, pregnancy, and overall side effects and choice of patient. When combined with CBT, the best outcomes are often seen for moderate to severe cases.
Digital and low-intensity interventions:

Internet-delivered CBT PT sessions: Very good improvement in accessibility and reduction waiting times through structured programs delivered online and supported by therapists.
Applications and self-help tools: Evidence is variable; however, high-quality guided programs yield much better outcomes than unguided apps.
Teletherapy: Well established and greatly increases the range into remote or underserved areas.
Regular movement and exercise : Regular movement and exercise are known somatic and lifestyle therapies for the continuous reduction of anxiety states and improvement of sleep.
Examples of anxiety relief tools are breathing, PMR, and yoga. Good sleep hygiene and proper regulation of circadian rhythms provide the foundation for resilience to affect and emotions.
Neurosurgery and newer techniques:
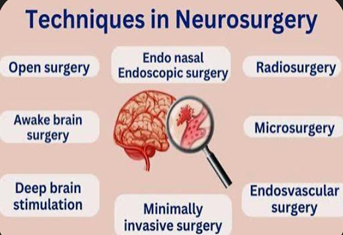
The FDA primarily approves Transcranial Magnetic Stimulation (TMS) to treat depression. New evidence shows it can also help with PTSD and treatment-resistant anxiety.
Somatic and lifestyle approaches: With somatic and lifestyle therapies, a person would have to exercise regularly and have movements that would keep reducing anxious states from time to time and improve sleep.
Anxiety has its instant reliefs like breathing exercises, progressive muscular relaxation, and yoga. Good sleep hygiene, combined with the regulation of the circadian rhythm, forms the bedrock of emotional resilience.
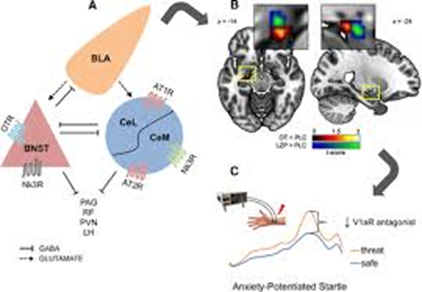
Neurosurgery and newer modalities:
Transcranial Magnetic Stimulation (TMS): Approved primarily for depression by the FDA, but there is new and promising evidence that supports it in PTSD and for a few cases of treatment-resistant anxiety.
In this regard, you said that, normally, a person who adopts his somatic and lifestyle therapies would need to exercise regularly and introduce movements that reduce anxious states on an ongoing basis and can promote better sleep.
Examples of anxiety relief tools would include breathing, PMR, and yoga. Good sleep hygiene and circadian rhythm regulation: The foundation of emotional resilience.
Neurosurgical approaches and newer modalities:
TMS is approved mainly by the FDA for depression, but there is new and promising evidence to support its use in PTSD and a few cases of treatment-resistant anxiety.
Somatics and lifestyle therapies : include the moving and exercising strategies that, day to day, gradually reduce anxiety states and improve sleep.
Breathing methods: progressive muscle relaxation, and yoga guide hands-on, pragmatic tools toward milking anxiety relief to the last minute.
The basic platforms for sleep hygiene and circadian rhythm regulation draw upon emotional resilience.
Neurosurgery and newer measures: TMS-Approved primarily by the FDA for depression; however, new and very promising evidence actually seems to migrate towards PTSD and a few cases of treatment-resistant anxiety.
Ketamine and esketamine: Rapid antidepressant effects whereas more keen interest is developing in severe, refractory PTSD and anxiety, used under specialist supervision.
Psilocybin and MDMA-assisted therapy: Currently undergoing clinical trials for PTSD and existential anxiety; very promising but very experimental and tightly controlled.
The future of tailoring care for generations to come:
Here are some shorter and more interesting formats: brief CBT modules, skills-focused but combined with some gamified apps that involve human coaching in psychoeducation, could trigger some interest for teens, or maybe even young adults.
Whole school approaches: incidence reductions and advantage-seeking are better among @ children with universal prevention (training for resilience, social-emotional learning).
Involvement of parents or partners: The most adherence is likely for systemic stressors when parents or partners are involved.
Adaptation of the interventions to culture-relative stigma and socioeconomic realities, both impacting access.
Prevention and Public health strategy Entry into schools and primary care at an early age could do a lot to prevent anxiety disorders from becoming chronic.
Public education campaigns related to normalizing help-seeking, as well as teaching basic coping skills (breathing, sleep hygiene).
Providing platforms within policy level supports like mental health services for students and flexible working conditions will create a buffered environment for reducing socioeconomic stressors.
For the Clinician, Caregiver, and Young Person:
Pragmatics
For clinicians, measurement-informed care, combination therapy where appropriate, and triage treatments to trauma-informed approaches.
Parents/caregivers should listen nonjudgmentally, encourage regular sleep and activity patterns, and de-emphasize punitive responses to avoidance behaviors; seek help early on in the professional help-seeking process.
For young people: A small, constant habits (like walking every day and establishing bedtime routines) do help. If anxiety is dangerous to life, talk to a trusted adult or professional in mental health: there’s good help out there.
Conclusion
Anxiety disorders, extending within a spectrum to almost never-ending worries to traumas rooted in PTSD, become determinative in the lives of most young people today. Technology, social pressures, global uncertainty, and changing cultural norms serve to modify the appearance of anxiety and its readiness for seeking help. Improvements have fortunately occurred in treatment options; evidence-based psychotherapies remain core to this modality, medication even though not frequently required enlarges utility, while digital tools and new biological approaches allow for broadening the toolkit. Identification early followed by trauma awareness and prevention at the community and school level may hence yield more hopeful outcomes in just minimizing burdens of anxiety for future generations.
Leave a Reply