Table of contents
The Unproven Link: Repetitive Head Trauma as Potential Cause
Facts and Figures on TBIs and Brain Tumors
Undergoing Treatment: Care Customization for the Athletic Body
Rehabilitation and this Pathway to Return to Play
Individualized Return-to-Play Protocols
Conclusion
Introduction
Diagnosing a brain tumor is challenging for anyone, but it is especially difficult for professional athletes. Moreover, putting up intense physical demands on their bodies, sports activities may pose one possible cause that might require these individuals to closely analyze the different treatments and the complex road to recovery, suffering from repetitive head trauma. This article provides a factual outlook, examining possible links between athletic activity and brain tumors, with meticulous attention to their specialized treatment and rehabilitation.
The Unproven Link: Repetitive Head Trauma as Potential Cause
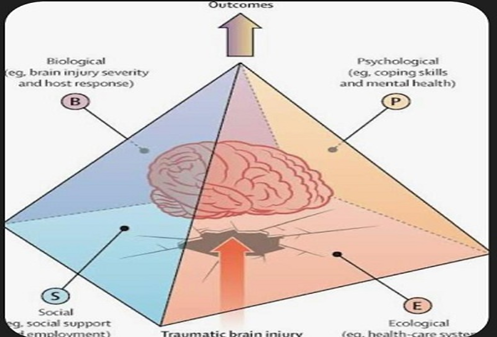
The etiologies for brain tumors mostly remain open; however, scientific interest appears to be growing regarding the possibility of trauma, particularly TBIs from repetitive head trauma common in contact sports, developing into subsequent brain tumors.
Facts and Figures on TBIs and Brain Tumors:

Post-Acute TBI Increased Risk: According to epidemiological studies, patients such as those with moderate to severe TBIs have been found to develop malignant brain tumors at a later stage of life. One of the largest studies, including more than 75,000 TBIs, showed that brain tumors occur more frequently than in uninjured controls. For instance, a study carried out in 2007 found, on average, that persons with a history of head injury have a 2.6-fold increase in odds of developing a brain tumor.
Biological Mechanism: Researchers are exploring the biological pathways involved in the link between head injuries and their effects, including inflammation, altered cellular signaling, and changes in the brain’s microenvironment. All these might induce specific brain cells, for instance, astrocytes, to go back to a more primitive, stem cell-like state and thus become more prone to carcinogenesis. University College London (2018) provided experimental evidence in mice that the co-occurrence of traumatic brain injury with the loss of a tumor suppressor gene could indeed initiate normal brain cells to a status associated with tumor-initiating cells.
Specific Tumor Types:
The link is strongest with gliomas, including glioblastoma, a highly aggressive form, and meningiomas, which may start as benign but carry an increasing risk of becoming malignant.
Beyond Injurious Factors: Beyond direct trauma, environmental exposures have also been speculated to play a role. A notable example was a Philadelphia Inquirer investigation (2013) that investigated the deaths of six former Philadelphia Phillies players from glioblastoma and believed to have had some correlation with the artificial turf at their erstwhile home stadium, Veterans Stadium. Such claims are not definitive, but they punctuate the complexity in identifying causes.
It is significant to mention that while these studies show a strong correlation between severe TBIs and increased incidence of some specific brain tumors, the absolute risk remains small. The majority of evidence from multiple studies continues to cause caution and further investigation, especially with athletes in high-impact sports.
Undergoing Treatment: Care Customization for the Athletic Body
An athlete receives treatment for a brain tumor exactly like any other patient, but supplemented with certain medical considerations needed to preserve both cognitive and physical functions critical to their profession. Surgery, radiation therapy, and chemotherapy are the main treatment modalities.
1. Surgical Intervention:
The basic objective of the surgery is the maximal safe tumor resection. It is especially delicate for athletes and needs much planning to minimize their neurological deficits.
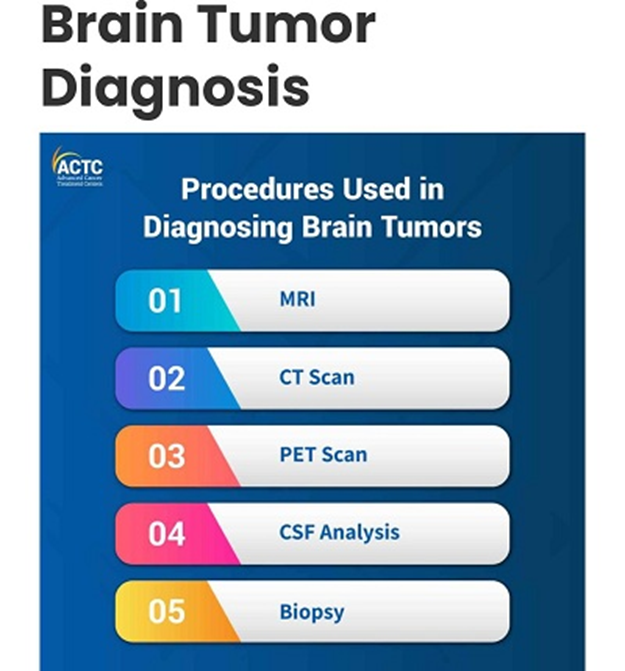
Craniotomy: This is the standard process of opening a part of the skull surgically to reach and remove a tumor.
Awake Brain Surgery: In some instances, especially in tumors located near critical functional areas (motor cortex, speech centers), the procedures can be performed awake by the surgeon. Parts of the surgery are done while the patient is awake to allow a real-time mapping of brain functions while being done by asking the patient to do tasks or answer questions. This technique allows the protection of the athlete’s area, controlling movements, coordination, and other abilities with respect to their sport.
Biopsy: a tumor’s location makes total resection unsafe, so doctors may perform a stereotactic biopsy to collect tissue for an accurate diagnosis and guide appropriate non-surgical treatments.
2. Radiation Therapy:
Radiation applies clinically high-energy beams directed against tumor cells or prevents their growth. It may serve as primary therapy or may follow the surgical process to eliminate remnant cells or provide palliation.
Targeted delivery: Modern radiation delivery methods, such as intensity-modulated radiation therapy (IMRT) and stereotactic radiosurgery (SRS), permit the delivery of high radiation doses to the tumor while sparing surrounding healthy brain tissue. This concern becomes more relevant in the case of the athlete, as this would allow some degree of prevention from side effects that could otherwise have compromised cognitive functioning or energy levels.
Side effects such as fatigue, cognitive changes, or hair loss may interfere with an athlete’s performance, and therefore, management of side effects in such cases has to be individualized.
These treatments act systemically by means of drugs that kill or inhibit the growth of cancers.
3. Chemotherapy: Chemotherapy can be given orally or through an intravenous infusion, reaching and affecting cancerous cells throughout the body.
Targeted therapy: Targeted therapy has very recently identified drugs programmed to destroy specific pathways or mutations in cancer cells. Compared to standard chemotherapy, they usually produce fewer systemic side effects.
Tumor Treating Fields (TTF): A new venture involving the interference of the division of cancer cells through alternating electric fields placed onto transducers on the scalp. A prime example is professional dodgeball player Michael Davies, whose amalgamation of surgery, radiation, and TTF device application successfully treated him for malignant gliosarcoma and serves as a testament that advanced treatments do bring hope to athletes who have remained cancer-free for over eight years.
Rehabilitation and this Pathway to Return to Play
After the post-treatment timetable of an athlete with a brain tumor, the intensive rehabilitation and the process of returning to play require serious consideration.
Comprehensive Rehabilitation: The athlete engages in extensive physical therapy to restore strength, balance, and coordination; occupational therapy may be needed to re-learn daily living skills; and speech therapy may or may not be involved in case cognitive or communication deficits exist. All these endeavors aim to restore pre-illness physical and cognitive functioning to the best degree possible.
Individualized Return-to-Play Protocols
Unlike concussed athletes who have a standard return-to-play status, any athlete recovering from a brain tumor will have their decisions made, almost on a completely one-on-one basis, by a multidisciplinary team including neurosurgeons, oncologists, neurologists, neuropsychologists, and sports medicine specialists. Important considerations are:
The type and grade of tumor involved.
The extent of tumor resection.
Consequences of treatment (no post-treatment seizures or neurological deficits).
Characteristics of sport and level of contact.
Neuropsychological tests for cognitive assessment.
Radiological stability (with no evidence of recurrence or growth of the tumor).
Doctors typically enforce a longer waiting period before returning to contact sports to protect the brain or surgical site and prevent re-injury.
The psychological and emotional support: The other part of the burden of brain tumor diagnosis and treatment lies on the psychosocial and emotional spectrum. They may often need psychological support in facing uncertainty, the change in their physical ability, and the acceptance of loss of their athletic career. Most feel that the forward activity, even if minimal, is psychologically liberating and assists in the healing process.
Inspiring Journeys: The public stories of athletes diagnosed with brain tumors, such as Jason Collins (an NBA player), who is right now under treatment for a brain tumor, and Maria Menounos (who is a TV presenter and sports journalist), who has recovered from a benign meningioma, bear testimony to the courage, resilience, and support systems required to confront, fight, and eventually triumph over such a debilitating disease, often going back to live productive and influential lives.
Conclusion
Brain tumors and professional sports are uniquely challenging. While the definite association between repetitive head trauma and tumor development is still undetermined, the evidence seems to suggest that a cautious approach is warranted. The treatment has to be extensive and individualized, with utmost importance on delicate surgical procedures and contemporary therapy modalities. There is a milestone, from diagnosis through treatment to recovery and a very possible return to play, representing the developments of medical science and the persistence of athletic spirits.
Leave a Reply