Table of contents
Underlying Importance of Early Diagnosis and Intervention
Comprehensive Clinical Assessment: A Multifaceted Approach
Management Strategies: Individualized and Holistic Approach.
Challenges and Future Directions
Future directions in the area will likely be centered on
Conclusion
Introduction
Child and adolescent psychiatry is complicated. It is an important area of mental health that considers illnesses related to emotional, behavioral, and developmental difficulties experienced by young people. This article elaborates on some of the major issues in clinical assessment and management of childhood psychiatric disorders. It aligns with the implicit topics raised by the title and cover image of the book.
Underlying Importance of Early Diagnosis and Intervention
The Relevance of Early Detection and Early Intervention
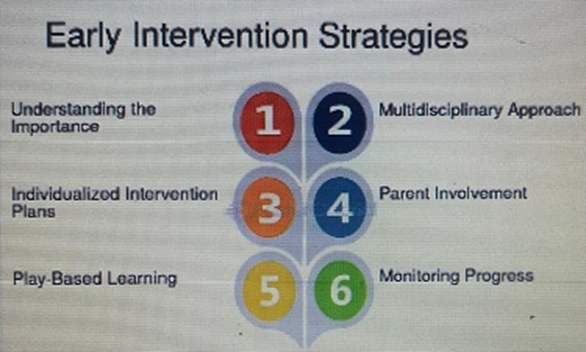
Childhood is a period of rapid development, and psychiatric disorders can enormously disrupt social, emotional, or cognitive growth. Identification and intervention are important for various reasons:
Developmental Trajectories: Unattended mental health concerns during childhood typically lead to more severe and persistent problems during adolescence and adulthood. For example, anxiety disorders in children can predispose them to anxiety and depression in adults, while early conduct problems can develop into antisocial personality disorder.
Brain Plasticity: Developing brains are more plastic or amenable to change. This plasticity can therefore be used to the advantage of interventions that may reshape some neural pathways and enhance healthier coping mechanisms.
Minimizing Functional Impairment: A psychiatric disorder in a child can negatively impact a child’s capability not only in education but also in making friends and participating in other activities. Through early intervention, a child’s functional damage can be prevented, allowing their abilities to be fully developed.
Family Impact: Child psychiatric disorders are stressors for the family. When a child is supported through proper management, it is also a crucial support for the family.
Comprehensive Clinical Assessment: A Multifaceted Approach
Management starts with a very thorough and holistic assessment. It is not solely about making a diagnosis but rather understanding the child in the context of his or her development, the family, social environment, and culture. Most assessments include:
Clinical Interview:
Child Interview: More age-appropriate techniques are used to get information directly from the child regarding his or her symptoms and feelings, thoughts, and experiences. This could include interviews by way of play therapy or art therapy for very young children.
The Parent/Caregiver Interview: Parents represent a child’s most valued resources on the developmental history, presenting complaints, family dynamics, medical history, and management in the past.
Teacher/School Personnel Interview: The school provides critical information regarding the child’s behavior, academic areas, and social interactions.
Developmental History: Developmental history presents sufficient detail of a child’s developmental milestones, including prenatal and birth history, motor development, language, social, and cognitive development. Any deviations or delays in any of these can be very significant pointers.
Medical History: Physical health, medicines, and past or present medical illnesses in the psychiatric context set the background in ruling out any underlying medical conditions that may mimic psychiatric symptoms.
Behavioral Observations: Observing the child directly across various settings (in the clinic, at home, and in school) adds some perspective on the child’s behaviors observed in real-time, fluctuations in moods, and social interaction, as well as gives information about coping styles that may have been developed by the child.
Psychological Testing: Standardized testing nowadays certainly provides objective indicators of cognitive abilities, for instance, traditional IQ tests, academic achievement, personality traits, as well as specific symptoms, which are similar to those on anxiety and depression scales. The results of these tools contribute to differential diagnosis and treatment planning.
Family Assessment: An assessment of the family’s structure, dynamics, communication, parental mental health, and stressors, all of which play a big role in the child’s well-being.
Analysis of Social and Environmental Factors: The peer relationships, school environment, community resources, cultural background, and any disturbing events or stressors are considered.
Management Strategies: Individualized and Holistic Approach.
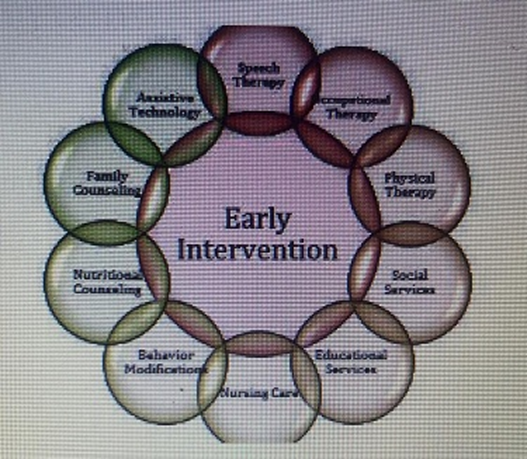
The management plan of childhood psychiatric disorders seldom lends itself to oversimplified one-size-fits-all solutions. It typically thrives on individualized integrated approaches that mostly constitute mixtures of therapeutic modalities.
There is this glowing image of a human brain on the book cover, and it subtly suggests such neurological feedback, consequently implying that therapeutic intervention is likely aimed at promoting an optimized functioning of the brain.
Psychotherapy:

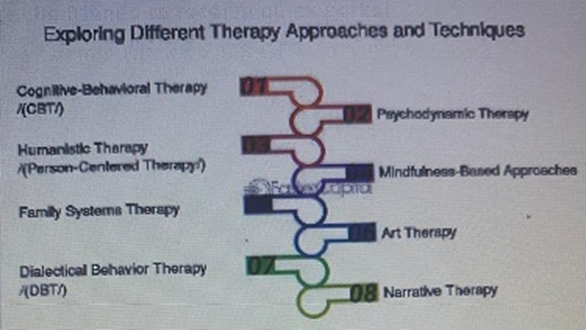
Cognitive Behavioral Therapy (CBT): CBT is a method used extensively to treat anxiety, depressive disorders, and obsessive-compulsive disorders. Accordingly, it goes along with a child’s detecting and changing of the unhelpful thoughts and behaviors.
Dialectical Behavior Therapy (DBT):
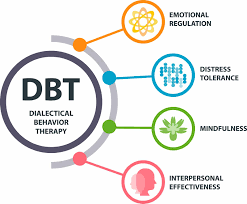
One-on-one DBT for teens aims at training the four core skills of emotion regulation, distress tolerance, interpersonal effectiveness, and mindfulness.
Play Therapy: At a child’s age, and mainly with very young children, play therapy may be a way through which children convey their feelings, go through their mood, and find solutions to the problems, all this while playing.
Family Therapy: This looks at issues related to family dynamics and works to enhance the communication between family members in order to pull together toward common strategies in helping the child.
Parent Management Training (PMT): Grants parents practical strategies to confront troubling behavior, also fostering positive interactions for strengthening the parent-child relationship.
Pharmacotherapy:
Medications should be considered whenever psychotherapy alone is insufficient to manage more severe symptoms or more specific disorders like ADHD, severe depression, anxiety, or bipolar disorder.
Consideration of consequences or benefits versus side effects should be undertaken, and the administration of pharmacotherapy should follow an integrated approach whereby it is combined with psychotherapy.
Another important aspect concerns dosage and monitoring, given that children and adolescents have rather distinct physiological characteristics.
Educational Interventions:
The involvement of schools is very much needed. This may include the creation of Individualized Education Programs (IEPs) or 504 plans that arm the child with accommodations, special education services, and behavioral support strategies within the academic context.
Similarly important will be dealing with any learning disability if it is expressed.
Social Skills Training: Social skills training helps several special children learn and practice appropriate social behaviors, communication, and problem-solving during peer interactions.
Lifestyle Interventions: Adopting healthy lifestyle features such as good nutrition, exercise, sleep, and reduced screen time would greatly benefit the encouragement of mental well-being, along with the treatment.
Collaboration and Coordination of Care: Management requires a multidisciplinary team of psychiatrists, psychologists, social workers, teachers, primary care physicians, and specialists as needed. For integrated care, communication should happen on a regular basis along with coordinated effort.
Challenges and Future Directions
Even though tremendous strides have been made, there still exist many challenges for child psychiatry, including:
Stigmas: The stigma of mental illness is seen to constitute a barrier to families seeking treatment.
Access to care: Trained child mental health professionals are scarce, and geographic disparities limit access to service provisions.
Diagnostic complexity: One of the biggest issues in identifying psychiatric problems in children is the fact that their development is vague and that they exhibit symptoms that can be seen in more than one disorder.
Dental research gaps: More research on the long-term effects of treatments and their effectiveness, especially in the cases of rare or complicated disorders, is urgently required.
Future directions in the area will likely be centered on
Precision Psychiatry: This type of treatment is based on an individual’s genetic, neurological, and environmental factors.
Digital Mental Health: Technology (apps, telemedicine) helps augment the number of patients that can be served and also facilitates driving the intervention.
Early Prevention Programs: In general, prevention and targeted prevention shall be the promoters of getting well and reducing the number of cases of the disorder.
Neuroscience Research: A stronger understanding of the neurobiology behind children’s psychiatric disorders will lead to developing more targeted and effective interventions.
Conclusion
In the case of Childhood Psychiatric Disorders, if you didn’t guess from the title and the imagery of a child’s mind glowing with activity, it embodies the high significance of knowing and treating mental health problems in children. With broad assessment strategies and the use of evidence-based management approaches, mental health clinicians are able to help children and adolescents who have serious mental illnesses become resilient adults and, along with the psychopath, have a better life. Future funding of research, education, and suitable care will be the key to guaranteeing that all children.
Leave a Reply