Table of contents
Denial Fears in Prior Authorization
Cohere Health Findings: Promise of AI
The Conflict: Trust in Technology vs. Trust in Payers
Denial Fears in Prior Authorization
The advent of Artificial Intelligence (AI) in the administration of health care services, especially prior authorization (PA), creates a notable difference in view between the likes of Cohere Health and major health technology companies and the major physician advocacy organizations in this industry, such as the American Medical Association (AMA). While Cohere Health’s survey data indicate strong provider trust and interest in AI-powered solutions that could reduce some administrative processes, the AMA’s study points to physicians’ concerns about the potential rise in denial rates due to AI use among health plans, with some arguing that such scenarios could lead to more harm to patients.
Cohere Health Findings: Promise of AI
Cohere Health announced the findings from its latest National Provider Survey on Prior Authorization for the year 2025. Despite some initial hesitations about the acculturated aspect of PA to AI, the survey provides a surprisingly positive view of provider sentiment toward AI in the PA process, significantly strengthening the understanding of this aspect. The study, which involved 200 clinicians and office administrators, found nearly universal confidence in AI-driven PA:
Clinician Confidence: 99% of clinicians expressed confidence in the artificial intelligence’s role in prior approval decisions.
Need for Digital Solutions: The findings further demonstrate overwhelming support for an entirely digitized prior approval process along with real-time tracking. Many providers are favorable towards the prospects that AI introduces to making the process smarter, simpler, and more transparent.
Efficiency Gains: Cohere Health’s platform claims that clinician-crafted AI models can auto-approve as many as 90% of requests every day, according to the AMA. Data: Payers’ AI peril resulting in a significant decline in turnaround time and administrative workload for provider staff.
These results suggest that many healthcare providers, increasingly frustrated with manual and complex PA systems, tend to view AI as a vital element in streamlining workflows, reducing delays, and ultimately making it faster for patients to gain access to desperately needed care. Cohere’s message is that their responsible, clinically trained AI augments clinical judgment rather than replacing it.
AMA Data: Payers’ AI Peril
The American Medical Association’s (AMA) annual surveys on prior authorization, on the other hand, describe a completely different world that concerns the menacing impact of the status quo and individual fears regarding the implementation of AI by health plans. The AMA’s 2024 survey of 1,000 practicing physicians revealed classic fears:
Concern about Increased Denials: More than half of the physicians, a three-fifths proportion of those surveyed, expressed concern that health plans’ use of AI will lead to increased denial rates for authorization. The cause for their fear stems from reports that some AI tools lead to very high rates of denial of care, in a few instances, far higher than the norm.
Adverse Effects on Patients: The strongest basis for the AMA’s resistance rests on patient harm. The data consistently show that prior authorization is delaying necessary care, as reported by 93% of physicians, and adversely affecting patients’ clinical outcomes, as reported by 94%. Disturbingly, greater than one in four, or 29%, of the physicians surveyed reported that prior authorization had led to a serious adverse event for a patient, which included but was not limited to hospitalization or death.
Administrative Burden: The AMA research reveals more than these named burdens. On average, physicians and their staff expend considerable effort, approximately 13 hours per week, on various tasks related to prior authorization, and these deep-rooted burdens contribute greatly to physician burnout.
View on the Use of AI: The leaders at the AMA emphasize that it is thus not acceptable to use AI for purely automatic denial of much-needed care. Instead, AI must augment human decision-making, rather than take over qualified clinical supervision in cases of denial.
The Conflict: Trust in Technology vs. Trust in Payers
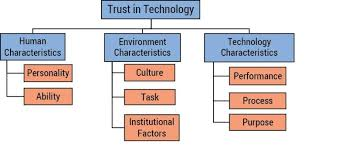
It is not the technology itself, but trust and implementation that turn core conflict:
Cohere Health Survey View of Feature
Provider Sentiment Towards AI: 99% confident in AI. 61% of respondents indicate that AI would increase denials.
Primary Purpose: Streamlining PA and increasing auto-approvals (up to 90%) and faster access to care. Reforming the PA process to eliminate wait time, harm, and burnout for patients and physicians.
Use of AI Automated approvals for routine, evidence-based care, with reserved use of human oversight for those cases with complexity, and insurers’ use of unsupervised AI to make denials in large batches without qualified human review.
The providers surveyed by Cohere Health seem to trust AI as a concept for its potential to listen to and understand the PA nightmare, especially within a system designed for clinical intelligence and high auto-approval. The affidavit members surveyed by the AMA, however, show a lot of guardedness against and in the future against the likely use of AI by health plans, as they see this being manipulated as an automated form of keeping a tight closure to even more patient care, rather than opening a wider door for them.
As the new CMS regulations take effect, requiring PAs to respond more quickly, the debate intensifies on how health plans will utilize AI, whether as an efficiency tool for collaboration or as a cost-cutting measure for denial.
Leave a Reply